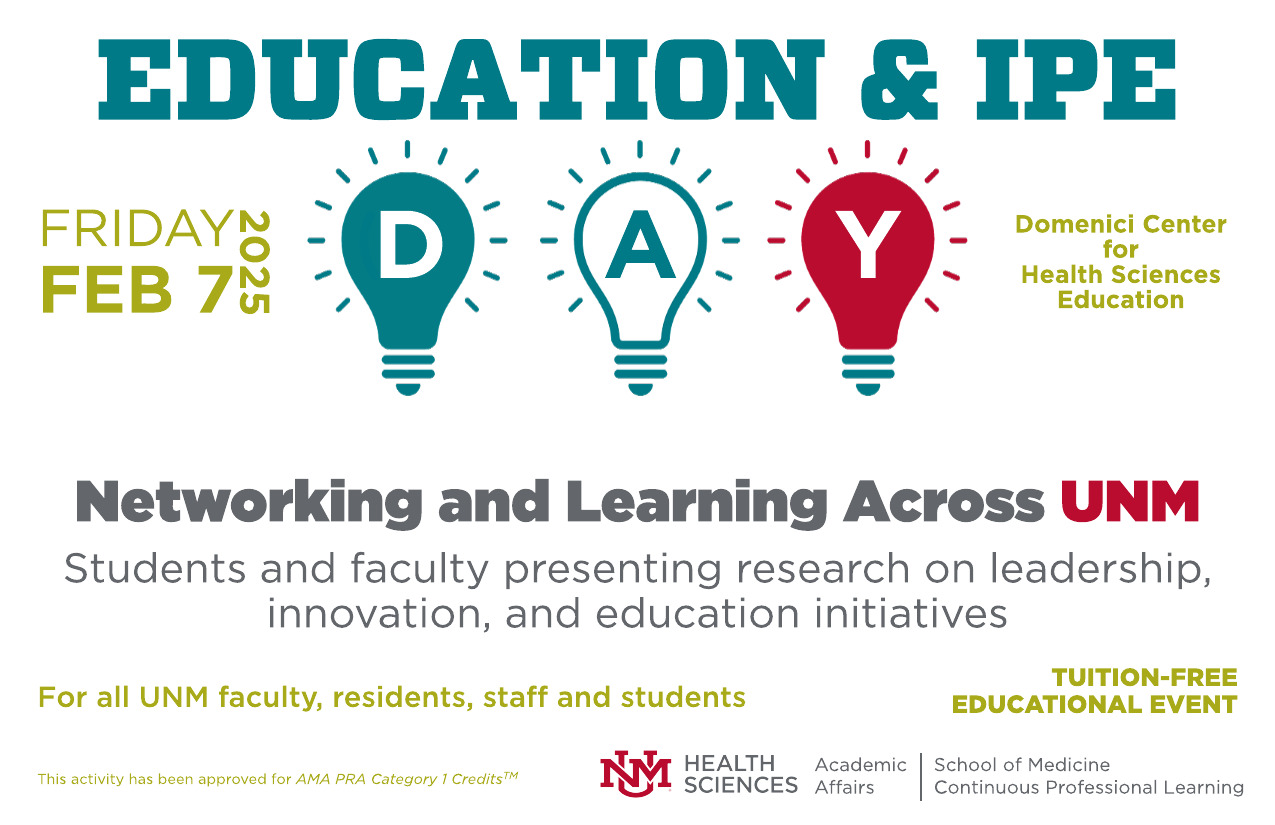
HSC Education Days
Minimizing the Squeeze, Maximizing the Juice: A Call for Efficiency in Resident Teaching
Document Type
Poster
Publication Date
4-29-2022
Abstract
BACKGROUND
Balancing clinical duties with education and personal well-being is one of the longest standing challenges in residency training. The COVID-19 Pandemic has tipped the scale even further in favor of centering on patient care, but at the expense of our personal wellness and education. In our 2020-2021 ACGME survey, “an appropriate amount of teaching in all clinical and didactic activities” was reported only 72% of the time, which is lower than the national average of 81%. Time is a scarce resource, limiting our ability to teach and to learn, but now this disparity is ever present. While we cannot fully anticipate the patient care challenges we will face in this new era of medicine, we can arm our trainees with the most valuable tool we have: education. We set out to improve resident education through a series of PDSA cycles.
METHODS
This is an ongoing medical education quality improvement study consisting of multiple PDSA cycles. PDSA cycle 1 consisted of a voluntary needs assessment to evaluate the strengths and opportunities in education within our residency program. PDSA cycle 2 involved the implementation of a resident workshop on efficient teaching techniques. The workshop contained an overview of 5 validated efficient teaching techniques, such as “arrow in the quiver,” “think aloud,” and “activated demonstration.” Participants were broken up into groups for skills practice and then reflected on how to incorporate these techniques into their daily workflow on inpatient wards.
RESULTS
The needs assessment was administered to 1st-3rd year internal medicine residents. The response rate was 40%. 56% of residents reported being satisfied with their education. Barriers to education were “lack of time” and not having an available teacher. Patient care, short teaching topics and “learning on the fly” were the top three ranked effective learning experiences. A common theme was a concern for clinical duties overpowering educational priorities. Overall, the pilot workshop was well attended and effective. There was an increase in pre and post workshop familiarity of each teaching method. Workshop strengths included that it was interactive, and contained skills practice and reflection.
DISCUSSION
While the majority of our residents are satisfied with the teaching they receive, we identified opportunities for improvement. Residents report two barriers to optimizing their education: time and access. Since time will always be in short supply, we anticipate a continued focus on training residents and faculty on efficient teaching techniques will be crucial. Next steps include soliciting faculty feedback and formally expanding the workshop to all residents.
Recommended Citation
Illescas, Alisa; Patrick Rendón; and Mary Lacy. "Minimizing the Squeeze, Maximizing the Juice: A Call for Efficiency in Resident Teaching." (2022). https://digitalrepository.unm.edu/hsc_ed_day/122
