Document Type
Article
Publication Date
8-12-2021
Abstract
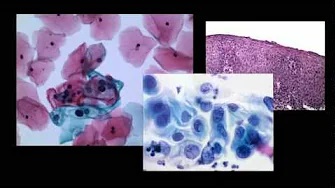
Pathogenic New World orthohantaviruses cause hantavirus cardiopulmonary syndrome (HCPS), a severe immunopathogenic disease in humans manifested by pulmonary edema and respiratory distress, with case fatality rates approaching 40%. High levels of inflammatory mediators are present in the lungs and systemic circulation of HCPS patients. Previous studies have provided insights into the pathophysiology of HCPS. However, the longitudinal correlations of innate and adaptive immune responses and disease outcomes remain unresolved. This study analyzed serial immune responses in 13 HCPS cases due to Sin Nombre orthohantavirus (SNV), with 11 severe cases requiring extracorporeal membrane oxygenation (ECMO) treatment and two mild cases. We measured viral load, levels of various cytokines, urokinase plasminogen activator (uPA), and plasminogen activator inhibitor-1 (PAI-1). We found significantly elevated levels of proinflammatory cytokines and PAI-1 in five end-stage cases. There was no difference between the expression of active uPA in survivors' and decedents' cases. However, total uPA in decedents' cases was significantly higher compared to survivors'. In some end-stage cases, uPA was refractory to PAI-1 inhibition as measured by zymography, where uPA and PAI-1 were strongly correlated to lymphocyte counts and IFN-γ. We also found bacterial co-infection influencing the etiology and outcome of immune response in two cases. Unsupervised Principal Component Analysis and hierarchical cluster analyses resolved separate waves of correlated immune mediators expressed in one case patient due to a sequential co-infection of bacteria and SNV. Overall, a robust proinflammatory immune response, characterized by an imbalance in T helper 17 (Th17) and regulatory T-cells (Treg) subsets, was correlated with dysregulated inflammation and mortality. Our sample size is small; however, the core differences correlated to survivors and end-stage HCPS are instructive.
Recommended Citation
Simons P, Guo Y, Bondu V, Tigert SL, Harkins M, Goodfellow S, Tompkins C, Chabot-Richards D, Yang XO, Bosc LG, Bradfute S, Lawrence DA, Buranda T. Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease. Viruses. 2021 Aug 12;13(8):1597. doi: 10.3390/v13081597. PMID: 34452463; PMCID: PMC8402847.