Document Type
Article
Publication Date
12-15-2023
Abstract
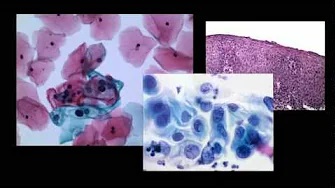
Chronic myeloid leukemia (CML) is characterized by leukocytosis with left-shifted neutrophilia, basophilia, eosinophilia, and variable thrombocytosis. However, extremely rare cases of patients with CML without significant leukocytosis and thrombocytosis (aleukemic phase [ALP] CML, or CML-ALP) have been reported. Due to its rarity and limited awareness, there remains a significant knowledge gap concerning the pathologic diagnosis, disease progression, and optimal patient management and outcomes. In this multi-institutional study, we investigated 31 patients with CML-ALP. Over half (54.8%) of patients had a history of or concurrent hematopoietic or nonhematopoietic malignancies. At time of diagnosis of CML-ALP, approximately 26.7% of patients exhibited neutrophilia, 56.7% had basophilia, and 13.3% showed eosinophilia. The median number of metaphases positive for t(9;22)(q34;q11.2) was 15, with a median of 38.5% of interphase nuclei positive for BCR::ABL1 by fluorescence in situ hybridization. The median BCR::ABL1 level was 26.14%. Remarkably, 14 (45.2%) patients were initially misdiagnosed or not diagnosed before karyotype or fluorescence in situ hybridization information for BCR::ABL1 became available. Twenty-five patients received tyrosine kinase inhibitors (TKIs). One patient developed blast crisis while on TKI treatment 8 months after initial diagnosis. With a median follow-up time of 46.1 months, 20 of 22 patients who received TKI therapy and had detailed follow-up information achieved complete cytogenetic remission or deeper, 15 achieved major molecular remission or deeper, and 10 achieved molecularly undetectable leukemia. In conclusion, given the frequent occurrence of prior or concurrent malignancies, aleukemic presentation, and low level of t(9;22)(q34;q11.2)/BCR::ABL1, misdiagnosis or delayed diagnosis is common among these patients. While these patients generally respond well to TKIs, rare patients may develop blastic transformation. It is therefore important for pathologists and hematologists to be aware of this highly unusual presentation of CML to ensure timely diagnosis and appropriate management.
Recommended Citation
Rivera D, Cui W, Gao J, Peker D, Zhang QY, Dewar R, Qiu L, Konoplev S, Hu Z, Sasaki K, Hu AY, E S, Liu M, Fang H, Wang W, Tang G, Apperley JF, Hochhaus A, Cortes JE, Khoury JD, Medeiros LJ, Jabbour E, Hu S. Aleukemic Chronic Myeloid Leukemia Without Neutrophilia and Thrombocytosis: a Report From the BCR::ABL1 Pathology Group. Mod Pathol. 2023 Dec 15;37(2):100406. doi: 10.1016/j.modpat.2023.100406. Epub ahead of print. PMID: 38104892.