Document Type
Poster
Publication Date
3-31-2023
Abstract
Background
Healthcare systems continuously strive to improve quality and value of the care. Advances in surgical technologies, enhanced perioperative surgical planning, and multidisciplinary care strategies are increasing the number of elective procedures in the geriatric population. However, frail older adults are more still likely to have poor postoperative outcomes. We examined the discriminative thresholds for the risk analysis index (RAI), modified frailty index-5 (mFI-5) and increasing patient age for predicting adverse postoperative outcomes.
Methods
Octogenarian neurosurgery patients undergoing spine, cranial, and other procedures, captured in the ACS-NSQIP between 2012-2020 were included. We employed receiver operating characteristic (ROC) curve to examine the discriminative thresholds of RAI, mFI-5, and increasing patient age. Multivariable analyses were performed. Our primary outcomes were 30-day mortality, extended length of stay (eLOS [≥75th percentile]) and continued inpatient care >30 days (pLOS). Secondary outcomes were skilled care facility (SNF) discharges and readmissions.
Results
20,710 octogenarians were included, with a mean age of 83 years (SD, 2.5), and a male (52.7%), and white (79.8%) majority. The RAI had higher predictive discriminative thresholds for 30-day mortality (C-statistic of 0.743), eLOS (C-statistic: 0.692), and pLOS (C-statistic: 0.665) compared to the mFI-5 (C-statistic: 0.574, 0.556, and 0.523 respectively), and increasing patient age (C-statistic: 0.577, 0.546, and 0.513 respectively), P<0.001. On multivariable analyses, RAI showed a larger effect size with adverse postoperative outcomes by increasing frailty strata than mFI-5 and increasing patient age. Nonetheless RAI showed decreased risk for SNF discharges.
Conclusion
We found that RAI was a more accurate predictor than mFI-5 and increasing patient age for mortality, eLOS, and pLOS in octogenarian neurosurgery patients. More research is needed on RAI’s performance in different specialized neurosurgical populations. It is increasingly clear that comprehensive risk assessment strategies tailored to optimize perioperative care should be prioritized to potentially improve outcomes for this at-risk population.
Recommended Citation
Yocky, Alyssa; Oluwafemi Owodunni; Evan Courville; Syed Faraz Kazim; Meic Schmidt; Susan Gearhart; Naomi George; Diana Green-Chandos; and Christian Bowers. "The Risk Analysis Index Has Superior Discrimination Compared to the Modified Frailty Index-5 in Predicting Worse Postoperative Outcomes for the Octogenarian Neurosurgical Patient." (2023). https://digitalrepository.unm.edu/hsc-bbhrd/71

Comments
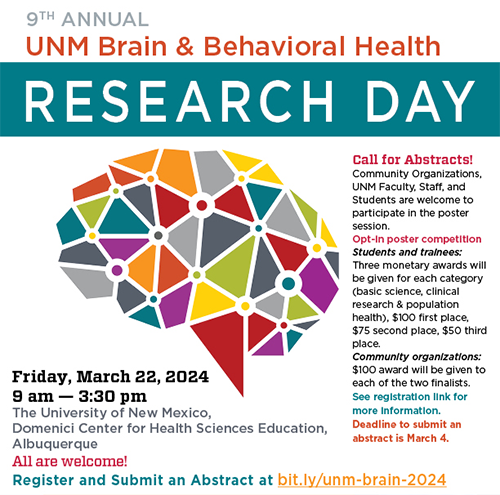
Poster presented at the Brain & Behavioral Health Research Day 2023