Document Type
Poster
Publication Date
3-31-2023
Abstract
Context: Access to medications for opioid use disorders (MOUD) is limited, especially in rural communities. Documented barriers limit integration of treatment for opioid use disorder (OUD) in primary care settings, inhibiting provider training and delivery of treatment. Innovative delivery mechanisms are needed to enhance integration of services.
Objective: Examine impact of participation in the Extensions for Community Healthcare Outcomes model (ECHO) intervention on expansion of OUD treatment using buprenorphine among rural primary care providers.
Study Design: Quasi-experimental single group design to assess achievement of benchmark measures related MOUD expansion.
Analysis: We estimated the strength of the association between participation in MOUD-focused ECHO sessions and expansion of MOUD treatment using logistic regression. Setting: Rural primary care providers in New Mexico and border areas in surrounding states (TX, AZ, CO). Population Studied: Medical Doctors, Doctors of Osteopathic Medicine, Nurse Practitioners, and Physician Assistants. Intervention/Instrument: A 12-session curriculum using the ECHO model providing education, support and consultation on key areas to help start and expand buprenorphine treatment including details on prescribing, psychosocial treatment, recovery support, and clinic functioning.
Outcome Measures: Primary outcome measures were the following MOUD implementation benchmarks: 1) obtaining DATA 2000 waiver, 2) obtaining license X number, 3) prescribing buprenorphine to first patient, 4) adding additional patients onto provider’s buprenorphine panel.
Results: We detected a positive relationship between participation in the ECHO and expansion of MOUD treatment. Specifically, there is a positive relationship to achieving any of the above benchmarks 1-5 (p<.001), and in particular the benchmark of starting to prescribe buprenorphine (p=.003). Participation: 81 prescribers across 49 clinics in rural areas of NM, CO, and TX participated in the study. Sixty-five percent (53/81) advanced to accomplish at least one benchmark, and 47% (38/81) have started adding additional patients to their buprenorphine panel.
Recommended Citation
Salvador, Julie; Snehal Bhatt; Vanessa Jacobsohn; Larissa Lindsey; Heidi Rishel Brakey; Rana Alkhafaji; Jesus Fuentes; Magdalena McWethy; Laura Rombach; Rachel Abeyta; Julia Martinez; Andrew Sussman; and Orrin Myers. "Participation in ECHO is Associated with Expanding Buprenorphine Treatment for Opioid Use Disorder in Rural Primary Care." (2023). https://digitalrepository.unm.edu/hsc-bbhrd/132



Comments
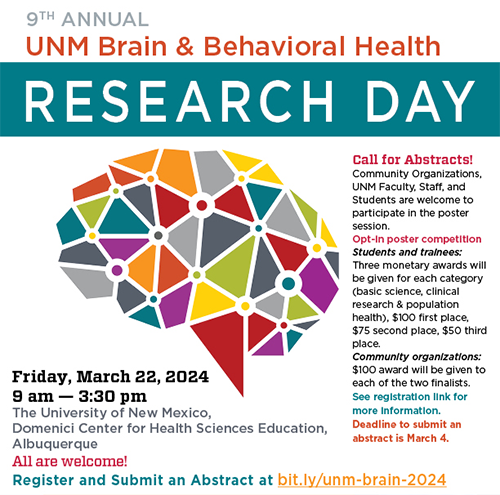
Poster presented at the Brain & Behavioral Health Research Day 2023